Introduction to article publication
The article was published in JAMA Internal Medicine ( IF: 20.768 ) on October 21, 2019 by Associate Professor Wang Yanyan, Master 's Tutor, West China Nursing School, Sichuan University.
Part I Interpretation of article content
Background
Postoperative delirium (POD) is one of the most common complications for older patients, which is associated with serious adverse outcomes, including increased length of hospital stay (LOS), mortality, risk of functional decline, and subsequent dementia. Previous studies have demonstrated that 30% to 40% of these cases are preventable. Currently, multicomponent non-pharmacological interventions are considered the first-line approach for delirium prevention. Among these approaches, the Hospital Elder Life Program (HELP) is the most widely implemented evidence based model that targets multiple risk factors for delirium. In 2013, HELP protocols were adapted to align with the National Institute for Health and Care Excellence (NICE) guidelines. In this study, they implemented a total of 11 protocols, comprising the original 6 volunteer-based HELP protocols, 2 original nursing-based HELP protocols, and 3 NICE guideline-adapted protocols. Furthermore, they tailored the protocols to address each patient’s risk factor profile so that each patient received a customized menu of interventions. To implement the program at their hospital, they adapted HELP to the Chinese culture. The innovation in this present study was called t-HELP (tailored, family-involved HELP), which involved family members instead of volunteers and applied a tailored approach to assigning HELPprotocols. The overarching rationale for the trial was to adapt HELP to local circumstances in China and demonstrate its effectiveness in a different health care system.
Study Design and Participants
A 2-arm, parallel-group, single-blind, cluster randomized clinical trial was conducted.
The study was carried out in 6 surgical floors—gastric, colorectal, pancreatic, biliary, thoracic, and thyroid. Patients aged 70 years or older and scheduled for an elective surgical procedure with an anticipated LOS longer than 2 days were eligible for inclusion. Exclusion criteria included (1) delirium at baseline as assessed with the Confusion Assessment Method(CAM); (2) a terminal condition with life expectancy of less than 6 months (eg, metastatic cancer, pancreatic cancer, or receiving end-of-life care); (3) inability to perform cognitive tests because of severe dementia, legal blindness, or severe deafness; (4) a documented history of schizophrenia or psychosis;
and (5) a documented history of alcohol abuse or withdrawal within the past 6 months and/or reporting consumption of more than 5 drinks per day for men (4 for women).
Interventions
Combined with China's cultural background and hospital resources, this research innovatively developed an individualized inpatient life support protocols (t-HELP) for the elderly with family participation based on the HELP program. The t-HELP protocol replaces the volunteers in the original protocols with family members or nursing workers to assist in completing part of the intervention protocols, which includes 3 general protocols and 8 individualized protocols (Figure 1 and Figure 2). The study adopted family education to help family members understand the importance of the intervention. Nurses supervised the implementation of the intervention and recorded the reasons for the non-compliance of the family to ensure the family’s compliance with the program.
In this study, patients who meet the criteria were divided into conventional group (receiving conventional treatment and nursing) and experimental group (receiving the
tailored HELP protocol daily from postoperative day 1 to postoperative day 7 or discharge) according to the ward grouping. After the intervention, the differences in the incidence of delirium, physical function, and cognitive function between the two groups were compared.
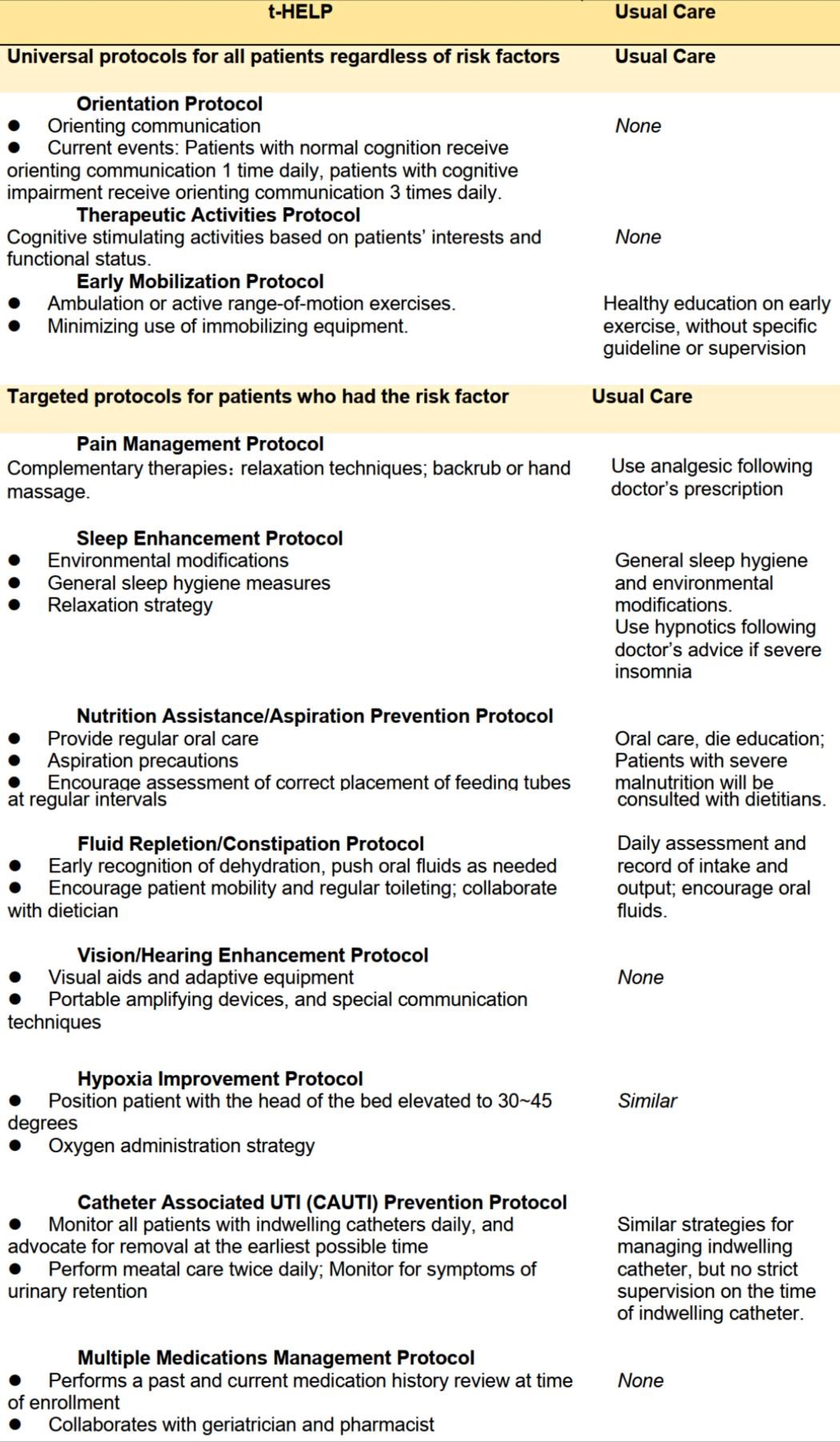
Figure 1. Differences of t-HELP and Usual Care
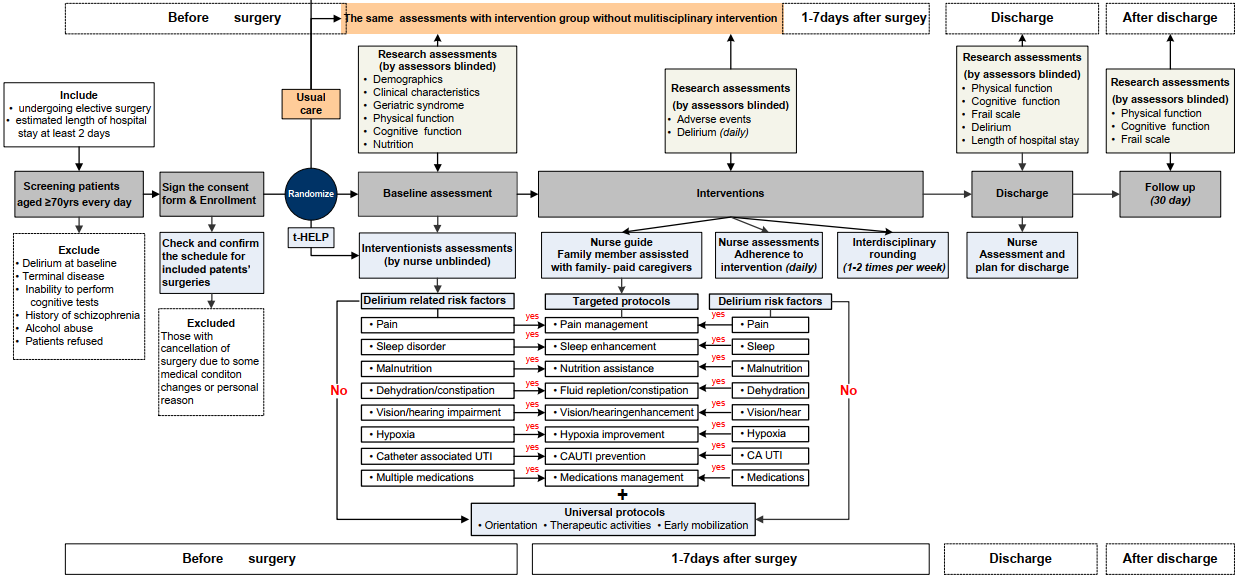
Figure2. Implementation Procedure
Statistical Analysis
SPSS, version 19.0 (IBM)was usedfor all statistical analyses,with 2-tailed tests as appropriate, and 2-sidedP<0.05 considered to be statistically significant. Participants’ baseline characteristicswere comparedusing an unpairedttest or, if the variables were not normally distributed, the Mann-Whitney test.The χ2 or Fisher exact testwasused for categorical or rankedvariables. Toaccountforthehierarchical structureofthedata (i.e., studyparticipants nested within nursing units),multi-levelbinomial regression modelwasused to estimate the effect of treatmenton primary outcome(PODincidence).A generalized estimatingequationwasbuilttoexaminetheassociationbetweenintervention and secondary outcomes (ADLs, IADLs, FRAIL score, andSPMSQ level before the operation, at discharge, and 30 days after discharge).
Results
Of the 475 patients screened for eligibility, 281 (171 [60.9%] male, mean [SD] age
74.7 [5.2] years) were enrolled and randomized to receive t-HELP (n=152) or usual care(n=129). PODoccurred in 4 participants (2.6%) in the intervention groupand in 25 (19.4%) in the control group, with a relative risk of 0.14 (95% CI, 0.05-0.38).The number needed to treat to prevent 1 case of POD was 5.9 (95% CI, 4.2-11.1). Participantsin the intervention group compared with the control group showed less decline in physicalfunction (median [interquartile range] for ADLs: -5 [-10 to 0] vs -20 [-30 to -10]; P<0.001;for IADLs: -2 [-2 to 0] vs -4 [-4 to -2]; P<0.001) and cognitive function (for the SPMSQ level:1 [0.8%] vs 8 [7.0%]; P = .009) at discharge, as well as shorter mean (SD) LOS (12.15 [3.78]days vs 16.41 [4.69] days; P<0.001).
Conclusions
The findingsof this studysuggest that t-HELP, with family involvement atits core, is effective in reducing POD for older patients, maintaining or improving theirphysical and cognitive functions, and shortening the LOS.This exampleof t-HELP implementation may provide ideas to hospitals interested in instituting HELP on how they can launch theinterventions using existing staff and resources. The t-HELPtrial may improve the generalizability and increase the implementation of HELP.
Limitations
This study has some limitations. First, despite all efforts to maintain blinding, blinding might have been compromised in some situations owing to the nature of the research (e.g., we could not double-blind because t-HELP patients and staff were aware of the interventions) and to potential subjective contributions to some of the outcome ratings (e.g., delirium, function). These circumstances may have led to the overestimation of the effect of t-HELP. Second, the 7-day duration of the intervention was shorter than the mean LOS. This duration was chosen to balance the peak days of delirium onset in the population (POD 3-5) against the practical constraints of the study resources. Third, the enrollment rate of men is higher than that of women, but no significant effect of sex on the incidence of POD was observed. Fourth, because of feasibility constraints, they were unable to assess the long-term effect of t-HELP on cognitive or physical functioning, which remains an important area for future research.
Part II Guiding Significance of Research Results to Practice
The results showed that the individualized and family-involved t-HELP, could prevent POD in elderly patients, maintain postoperative physical and cognitive function in elderly patients with surgery, and shorten the average length of stay. Based on the Chinese characteristics of elderly care culture and the existing resources of Chinese hospital system, the t-HELP innovatively integrates family members or caregivers to assist in the implementation of intervention programs. It is an extension and application of the traditional HELP, and it also provides evidence-based evidence for medical institutions with similar cultural backgrounds in the world to prevent senile delirium in the elderly.
Part III Peer Expert Reviews
1) The team of Victoria Tang, Emily Finlayson and Kenneth Covinsky of the University of California, San Francisco made comments on the same period, affirming the innovation of this research, and calling for American hospitals to learn from other cultures and include family members and caregivers in hospital patient treatment plans. The comment pointed out that the American medical community has gradually realized the need to improve the healthcare system and encourage family members and caregivers to actively participate in family care. In 2016, the perioperative consensus guidelines issued by the American College of Surgeons and the American Geriatrics Society also emphasized the importance of family members and caregivers’ involvement in intervention treatment. Long-term trust in family members or caregivers may help increase the patient's sense of security during hospitalization, encourage early getting out of bed, reduce anxiety and enhance sleep quality. Family members can effectively mobilize patients to actively participate in the whole process of rehabilitation based on their understanding of patients' daily habits and cultural background.
Kenneth Covinsky,Professor of Geriatrics, University of California, San Francisco. Chief Fellow, UCSF Older Americans Independence Center, University of California, San Francisco. Deputy Editor-in-Chief of JAMA-Internal Medicine. Director of Department of Clinical Aging, National Institute on Aging. His main research interest is elderly disability, and he proposed that functional status is an important factor in determining the health status and quality of life in the elderly. He was awarded Edmund G. Brown, Sr Senior Professor of Gerontology, and won the National Research Tutor Award.
2)Professor Hu Xiuying: This is a successful demonstration of medical-nursing cooperation. Effective care of medical-nursing cooperation plays a key role in the countermeasures to the health problems of the elderly. At present, there is no specific assessment systems and intervention protocols for perioperative delirium in China. The multidisciplinary team of delirium in this research took the lead in establishing a multidisciplinary comprehensive intervention mode t-HELP for perioperative delirium in the elderly of China, which is an extension and innovation of the HELP. It is also a useful attempt to put the theory of geriatric medicine into clinical application, improve the safety during the perioperative period, and optimize the quality of care for elderly surgical patients. In addition, the multidisciplinary collaboration mode involving clinical nurses will play a good role in promoting the development of the nursing discipline and the advantage and initiative of the nursing team.
Hu Xiuying,Doctor of Nursing, Professor, Doctoral Supervisor. Director of West China Nursing Innovation Research Center, West China School of Medicine/West China Hospital, Sichuan University, former Dean of West China School of Nursing and former Director of Nursing Department of West China Hospital, Sichuan University,. She is an academic and technical leader, health and family planning leading talent in Sichuan Province, a member of the Discipline Evaluation Group of the Degree Committee of the State Council, a member of the National Medical Postgraduate Education Steering Committee of the Ministry of Education, Vice Chair of the Geriatric Committee of the Chinese Nursing Association, Chair of the Geriatric Committee of Nursing Association of Sichuan Province, and Chair of the Chengdu Nursing Association. Her main research interests are geriatric nursing and disaster nursing, and she has cultivated more than 30 PhD and master students (Wang Yanyan is one of the outstanding doctors). She has published more than 150 papers, edited more than 10 textbooks/monographs, and been in charge of more than 10 scientific research projects. Furthermore, she has won 6 science and technology awards, 7 patents, 1 scientific research innovation team of the Education Department of Sichuan Province, and the titles of "the sixth National Excellent Scientific and Technological Worker" and "National Excellent Director of Nursing Department".
Part IV Introduction to Corresponding Author, First Author and Research Team
Corresponding Author:Yue Jirong,Doctor of Gerontology, Professor, Doctoral Supervisor, Vice Director of Department of Geriatrics. She once went to the Hebrew Geriatrics Center of Harvard Medical School to conduct research on cognitive dysfunction and delirium in September, 2012. Her research interests cover senile frailty, senile delirium and perioperative evaluation. She is a committee member of the Neurology Group of the Geriatric Medicine Society, Chinese Medical Association, a standing member of Geriatric Committee of Chinese Geriatrics Society, Vice Chair of Smart Medical and Elderly Care Association of Chinese Geriatrics Society, and Vice Chair of the Sichuan Medical Doctor Association for Geriatrics. She has published more than 80 papers (including more than 20 SCI papers as the first or corresponding author, and 2 ESI highly cited papers), and she wrote theChinese Expert Consensus on Prevention and Control of Elderly Patients with Postoperative Delirium. She has been in charge of and participated in a number of national and provincial-level scientific research projects, such as national key research and development projects, national Nature Science Foundation of China projects, and international collaborative projects of Harvard University. She has translated as the chief translator, edited and co-edited 8 textbooks and monographs. In addition, she was awarded the second prize of Sichuan Science and Technology Progress Award in 2017.
First Author: Wang Yanyan,PhD of medicine/nursing, postdoctoral in Geriatrics, postdoctoral fellow at the University of Texas at Austin, Associate Professor at the National Center for Clinical Research on Geriatrics Diseases, West China Hospital, Sichuan University. Her research interest covers cognitive function and sleep disordered breathing in the elderly. She is in charge of 1 national Natural Science Foundation of China Youth Fund project, 1 provincial Science and Technology Department project, 2 provincial Health and Family Planning Commission projects, and she participates in two national research projects as the lead researcher. During post-doctoral study in the United States, she participated in two NIH studies on drug intervention, one is CPAP intervention in elderly sleep apnea to improve cognitive function, and the other is nocturnal restlessness and restless legs syndrome in nursing homes with Alzheimer’s disease. She has published 5 articles in SCI, 4 articles in MEDLINE and more than 10 articles in Chinese core journals as the first author. In addition, she has also published 12 articles in SCI, 1 article in MEDLINE, and 8 articles in Chines core journals as the second author or other author in type. She has made oral presentations or posters at the American Delirium Association Annual Meeting (2015), Delirium HELP Annual Meeting (2017), American Sleep Medicine Association Annual Meeting (SLEEP 2018 and SLEEP 2019), and Southern Society for Nursing Research (SNRS 2019).
Team Introduction
The elderly delirium multidisciplinary team of West China Hospital, Sichuan University, is the same team as the elderly ACE ward. While diagnosing and treating acute diseases, they focus on and address all risk factors affecting return to ' healthy ' life in the elderly, including nutritional status, physical activity, cognitive function and a series of geriatric syndromes. They pay special attention to the maintenance of cognitive and physical function of the frail elderly. Team members include geriatric medical and nursing experts, therapists, clinical nutritionists, clinical pharmacists, etc. They have applied for more than 10 research projects, and published more than 20 papers in the diagnosis, early warning, intervention, and mechanism research of delirium. At present, they are committed to promoting the intervention mode of multidisciplinary cooperation for the frail elderly to improve their mobility and function, so that they can maintain their self-care ability and activity status.